Facts & Figures




Complex processes have made claims denial management increasingly difficult. In the past, denials management investments have focused on human capital solutions, while the development of technology and process improvements have been lagging. Even with new denials tactics in place, healthcare organizations are struggling to keep pace. They are finding it challenging to implement long-term process changes and deploy personnel effectively to prevent denials. Additionally, unknown financial implications have resulted in acceptance rather than process enhancements or change management.
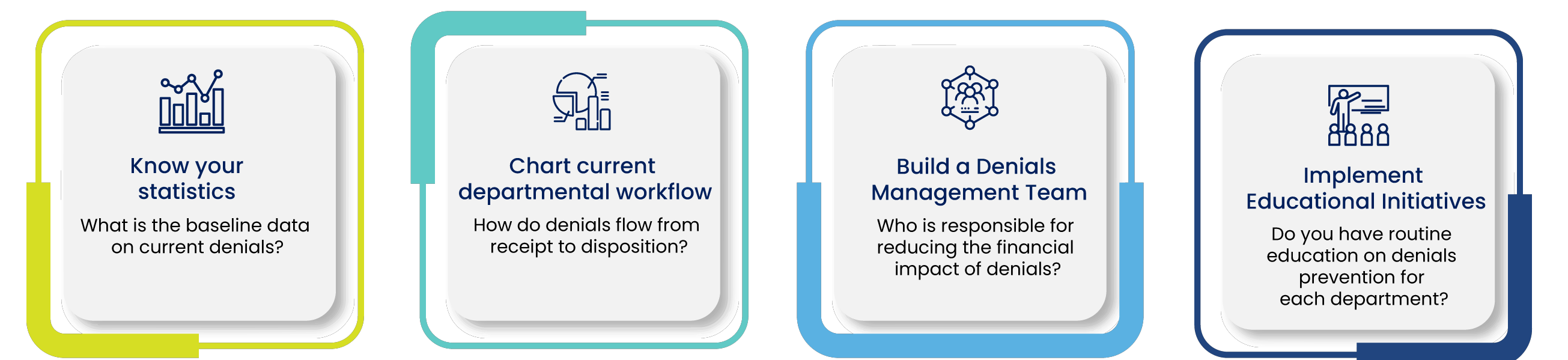
What is the Solution
How Innova Can Help
We provide healthcare organizations with a comprehensive denials management solution that encompasses three primary areas of focus— technology and analysis, a solutions-based approach, and an emphasis on outcomes. As we continually check the data and analytics and determine the root cause, we also help the healthcare stakeholders to identify where the denials are occurring in the revenue cycle. This approach helps us to zero in on solutions tailored to the organization’s unique needs. Continuing to prioritize the outcomes our team concentrates on sustainable process improvements that lead to improved financial outcomes and an enhanced care continuum.

Why Innova
Years of experience
Experts in Denials Management
clients have entrusted us with part or all of their denials management process
With the right blend of empowered front-line staff, optimized processes, and integrated technology, we will ensure that you reduce the number of denials. As we draw on the expertise of our professionals who have an in-depth understanding of denials management, we will reduce cash flow bottlenecks and improve your bottom-line.
By collaborating with us you will benefit from:
Streamlined workflows that lead to higher efficiencies, faster appeals, and uninterrupted cashflows.
Useful and specific recommendations for edit improvements, process improvements, and claim management.
Services that reduce regulatory risks and improve compliance.
System-agnostic solutions that resolve the issue of underpayments.
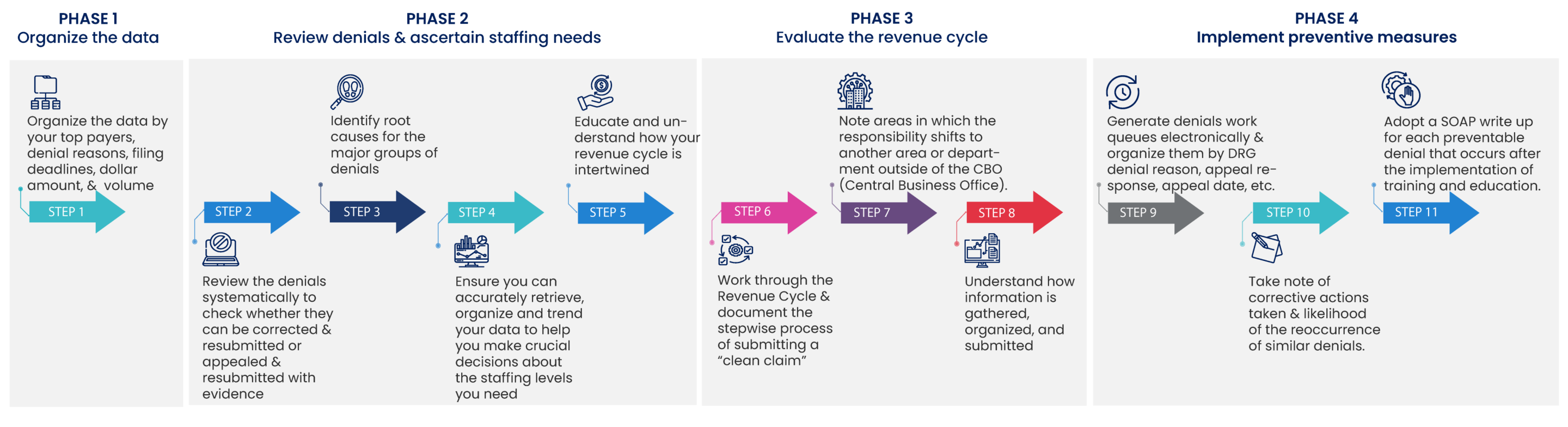
The business model that we follow:
Select team from
our pool of
experienced talent
Integrate our denials management team into your revenue cycle process
Install analytics
package to:
- Identify trends
- Recommend education
- Prevent future denials
Once the Innova team is on board they will manage all denials
- Determine root cause analysis for each denial
- Implement corrective action, if possible
- Track: appeal rate, timely filing deadlines, root cause, corrective actions
Our Approach
Our Denials Analytics Platform

Related Services
Reports for Assessment
Appeals Management
Compliance & Security
Meet Our Leaders

Kelly Walton
Executive Director of Healthcare Operations